In the past few decades, rapid diagnostic tests have become an important tool in the global effort to control malaria. The relatively affordable test strips have identified millions of cases in just minutes, speeding up access to life-saving treatment. They’ve also significantly improved surveillance in harder-to-reach rural areas, giving public health experts a better understanding of the impact of this mosquito-borne disease that kills about half a million people worldwide each year.
But this progress may be threatened by the parasite that causes malaria.
Changes that make Plasmodium falciparum undetectable by the current gold-standard rapid test are spreading in many countries, leading to false-negative test rates as high as 80 percent in some hospitals. Although the prevalence of the changes is usually not that high, scientists are concerned that they could be spreading without notice, resulting in possibly hundreds of thousands of cases of this deadly disease going undetected, and delaying treatment. Without the development of new tests, the changes could be a major obstacle to global eradication efforts.
“This is a major concern, on par with drug and insecticide resistance,” says Jane Carlton, a biologist and director of Johns Hopkins Malaria Research Institute. “That's because it appears to be spreading.”
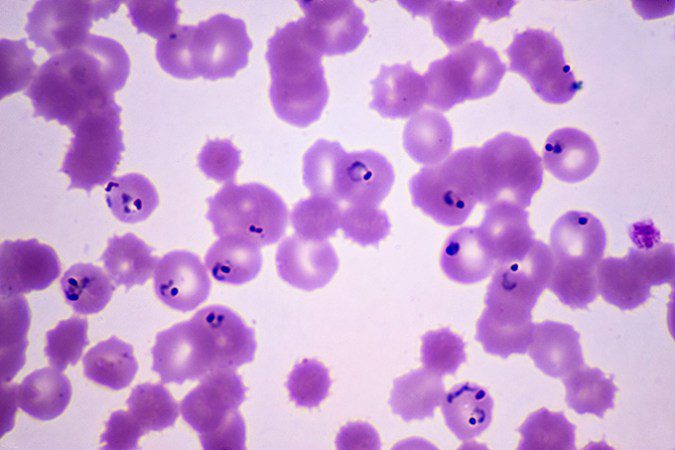
Scientists first reported these changes in 2010, after examining blood samples from patients in Peru. Although malaria parasites were present in the samples when viewed under the microscope, the rapid test results for the patients were negative. Most malaria rapid tests work by identifying P. falciparum histidine-rich protein 2 and 3, which are typically reliable signs of infection. However, researchers discovered that portions of the genes pfhrp2 and pfhrp3, which contain instructions for the proteins, had been removed from the malaria parasites in the Peruvian samples. The changes effectively masked the parasites from widely used rapid tests.
“This has a clear impact on our ability to diagnose and treat individuals,” says Oliver Watson, an infectious disease modeler at Imperial College London. Although there are alternative rapid tests that rely on other proteins, these tests are not widely used because they are “not quite as sensitive and a little more expensive,” Watson explains. As a result, the global supply of alternative tests is quite limited.
The test-evading changes have appeared in at least 40 countries across South America, Africa, and Asia. While many of the countries have reported barely any sign of the deletions, there’s evidence of rapid spread in certain regions, particularly the Horn of Africa (SN: 11/2/22).
In Eritrea, researchers began finding surprising numbers of false-positive rapid tests in 2014. Subsequent studies found that the parasites that could evade the tests were to blame. For example, at one Eritrean hospital, these parasites infected 21 out of 26 malaria patients — almost 81 percentAt another place, the parasites affected 10 out of 24 patients, which is about 42 percent. The high frequency led Eritrea to change its testing method to different rapid tests. Ethiopia and Djibouti, which also have high mutation rates that evade testing, have also begun using different tests.
According to some specialists, these efforts have mostly been successful. Microbiologist Michael Aidoo, associate director for laboratory science in the Division of Parasitic Diseases and Malaria at the U.S. Centers for Disease Control and Prevention, says, “There are no signs that the spread of mutations had a major impact on malaria control efforts, particularly due to the rapid detection and subsequent changes to test policies.”
In 2019, The World Health Organization published a reaction plan, recommending countries to change testing strategies when the prevalence of disguising mutations exceeds 5 percent. Determining whether this threshold has been reached in time to change testing strategies can be difficult.
“It’s not automatic to detect these mutant parasites,” says Carlton. It requires extensive testing of samples through more precise methods, such as microscopy or identifying the parasite by DNA, to confirm that a negative rapid test is actually positive and that the parasite contains mutations to evade the test. “It can be quite expensive to do that,” she says, so the quality of existing studies assessing the prevalence of these mutations, known as surveys, varies widely.
As a result, the global picture is still unclear in some areas.
“There’s a crucial need for more surveys,” Watson says. “Both to ensure that we have data from all malaria-endemic countries, but also to get more surveys in locations where we’re already seeing the mutations, to see how quickly they’re increasing.”
Within 20 years, 29 out of 49 malaria-endemic countries in Africa could have some areas that exceed the 5 percent threshold, as estimated by Watson and colleagues in a paper posted at medRxiv.org in January. East Africa, Senegal, and Mali are among the areas at highest risk, while Central Africa, which has the highest malaria burden, is at lower risk. The work hasn’t yet been peer-reviewed.
Currently available alternative tests will not be sufficient to meet this requirement, Watson says. More research is necessary to develop tests with higher sensitivity, “and we need a change from the manufacturing side, to ensure we have the [testing] capacity when countries need to switch,” he says.
If low-cost and precise alternative tests are widely accessible, this problem can be effectively managed, Watson says. But if they are not, it’s going to become much harder to control malaria in many countries. “It’s just an incredibly worrying problem.”