One day in March 2010, Isak McCune started clearing his throat with a forceful, violent sound. The New Hampshire toddler was 3, with a Beatles mop of blonde hair and a cuddly, loving personality. His parents had no idea where the guttural tic came from. They figured it was springtime allergies.
Soon after, Isak began to scream as if in pain and grunt at his parents and peers. When he wasn’t throwing hours-long tantrums, he stared vacantly into space. By the time he was 5, he was plagued by insistent, terrifying thoughts of death. “He would smash his head into windows and glass whenever the word ‘dead’ came into his head. He was trying to drown out the thoughts,” says his mother, Robin McCune, a baker in Goffstown, a small town outside Manchester, New Hampshire’s largest city.
Isak’s parents took him to pediatricians, therapy appointments, and psychiatrists. He was diagnosed with a host of disorders: sensory processing disorder, oppositional defiance disorder, and obsessive-compulsive disorder (OCD). At 5, he spent a year on Prozac, “and seemed to get worse on it,” says Robin McCune.
The McCunes tried to make peace with the idea that their son might never come back. In kindergarten, he grunted and screamed, frightening his teachers and classmates. “He started hearing voices, thought he saw things, he couldn’t go to the bathroom alone,” Robin McCune says. “His fear was immense and paralyzing.”
Other kids afflicted with PANDAS hear voices or experience “Alice in Wonderland” syndrome, wildly distorted perceptions.
As his behaviors worsened, both parents prepared themselves for the possibility that he’d have to be home-schooled or even institutionalized. Searching for some explanation, they came across a controversial diagnosis called pediatric autoimmune neuropsychiatric disorders associated with streptococci, or PANDAS. First proposed in 1998, PANDAS linked the sudden onset of psychiatric symptoms like Isak’s to strep infections.
They didn’t give it much thought. Periodic strep tests on Isak had always come back negative. And his symptoms seemed too dramatic to be the result of a simple, common childhood infection.
But as Isak’s illness dragged into its fourth year, they reconsidered the possibility. The year before the epic meltdowns began, his older brother had four strep infections; perhaps it was more than coincidence. In September 2013, three and a half years after his first tics appeared, a pediatric infectious-disease specialist in Boston put Isak on azithromycin, a common antibiotic used to treat food poisoning, severe ear infections, and particularly persistent cases of strep throat.
The results were dramatic. Isak’s crippling fear vanished within days. Then he stopped grunting. Less than a week after starting his son on the antibiotic, Adam McCune saw Isak smile for the first time in nearly four years. After a few weeks, the tantrums that had held the family hostage for years faded away.
Today, Adam McCune, a writer, likens the experience to welcoming his son back from captivity. “It’s like he was a POW for four years, and returned out of the blue one day,” he says. “To have my son back within a week was incredible.”
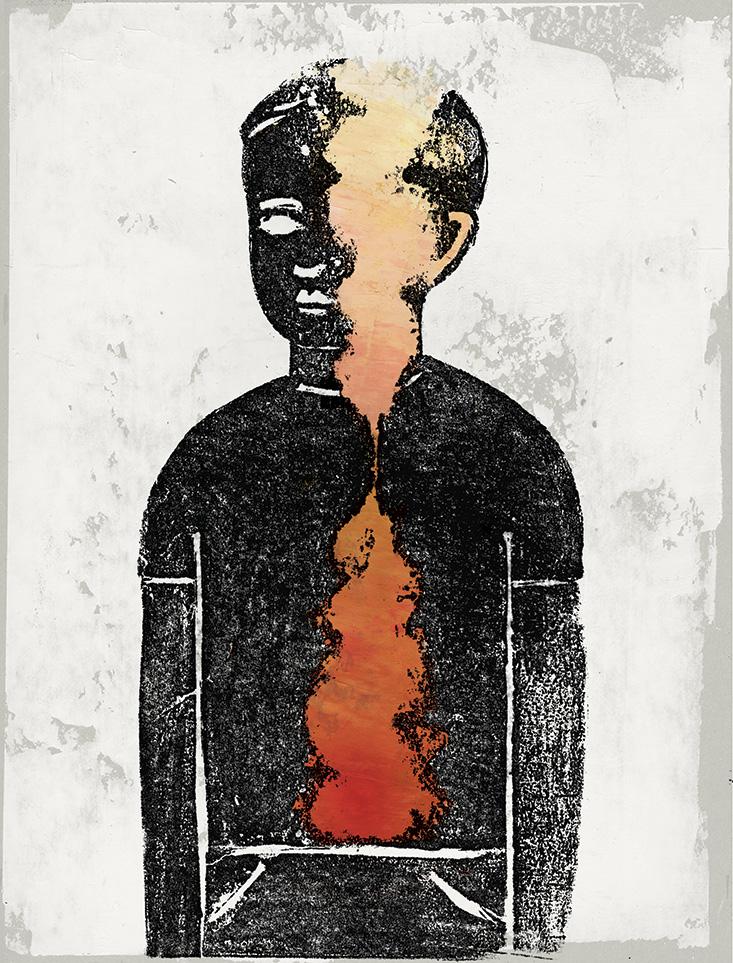
PANDAS represents a striking branch of medical research that has been gaining acceptance in recent years, though not without controversy. In a field known as immunopsychiatry, researchers are exploring the possibility that inflammation, or an overactive immune system, is linked to mental disorders that include depression, schizophrenia, and Alzheimers’ disease.
A host of recent genetic and epidemiological studies “have shown that when people are depressed or have psychotic episodes, inflammatory markers are found in their blood,” says Golam Khandaker, a senior clinical research associate at the University of Cambridge, in England, who studies inflammation and the brain.
In the case of PANDAS, when the body reacts to strep infection, parts of the brain that help regulate motion and behavior wind up caught in the crossfire, mistaken for bacterial invaders by cells bent on destroying them. Eliminate the inflammation, some doctors say, and you signal the immune system to stand down, restoring normal brain function.
The emergence of immunopsychiatry is a story of rediscovery, reflecting the twists and turns of mental health treatment over the last century. In the 19th century, mental illness and infectious disease were closely linked. That connection came uncoupled in the 20th century and immunopsychiatry’s argument that infection and inflammation can have a profound impact on the brain has struggled against psychiatric and neurological dogma. Yet emerging insights into mental illness unite the brain, body, and environment in ways that doctors and therapists are finally beginning to understand.
Nothing cemented the link between body and brain quite like syphilis. It was called “the disease of the century.”
In the 1880s, German psychiatrist Emil Kraepelin argued that mental illness and insanity were biological or genetic conditions. Kraepelin put a wide range of conditions under the umbrella term dementia praecox, or “premature dementia.” “He thought it was possibly linked with an infection somewhere in the body,” says Khandaker. In the pre-Freud era, Kraepelin’s classifications were tremendously influential.
At the time, nothing cemented the link between body and brain quite like syphilis, a sexually transmitted disease caused by the bacterium Treponema pallidum. Before antibiotics, a syphilis infection could be a slow-motion death sentence. In addition to ravaging the body, late-stage syphilis victims often escalated into what doctors at the time called neurosyphilis, a sort of manic, delusional state, before edging over into paralysis and death. It was a clear, common case of an infection causing psychosis.
Syphilis was so common it was called “the disease of the century.” Most patients were middle-class men; according to one estimate, 10 percent of patients in turn-of-the-century asylums were there because of neurosyphilis. “Syphilis strengthened the idea that infection and the immune system could be an important cause of mental illness,” says Khandaker.
Some potential syphilis cures even seemed to leverage the immune system. In the 1920s, an Austrian psychiatrist named Julius Wagner-Jauregg employed an unconventional syphilis treatment that would be condemned as unethical today. He deliberately infected late-stage syphilitics with malaria, hypothesizing that the ensuing immune response, including high fevers, might somehow burn syphilis out of the system. The treatment killed some but seemed to cure others, a result striking enough to earn Wagner-Jauregg the 1927 Nobel Prize in Medicine, the first ever awarded to a psychiatrist.
In a dramatic turn of medical history, the discovery of penicillin the following year led to our modern age of antibiotics and pushed diseases like syphilis out of the medical mind before the mechanism of Wagner-Jauregg’s cure was fully understood.
As antibiotics took hold in medicine, doctors increasingly treated the body and brain as separate entities. After WWII, Freud’s influence pushed the search for the roots of mental illness away from infection and disease and toward early childhood, family influence, and society. Autism was blamed on emotionally unavailable “refrigerator mothers,” OCD on overly strict toilet training, schizophrenia on harsh parenting styles. Depression was the result of childhood loss, or even an excess of parental love. Conversely, diseases we now know are infections—peptic ulcers, for example—were chalked up to stress and aggressive personalities. Most doctors and psychiatrists agreed that mental illness was all in the mind.
The growing influence of Freudian psychoanalysis coincided roughly with an understanding of the blood-brain barrier, a tightly woven net of tiny capillaries. The barrier acts as a fence between the circulatory system that supplies most of the body with blood and the brain’s cerebrospinal fluid, allowing nutrients and oxygen through but keeping blood cells—including immune cells—out. Its existence was hypothesized in the early 20th century and confirmed with the advent of electron microscopy in the 1960s. The blood-brain barrier led physicians to discount the possibility that the immune system’s antibodies might cause or contribute to mental illness. The brain was deemed “immunologically privileged.”
But it turns out the “blood brain barrier is not just not inviolate, it’s incompletely protective,” explains Mady Hornig, an epidemiologist specializing in neuropsychiatric disorders at Columbia University’s Mailman School of Public Health. “Parts of the brain are not protected at all, like the hypothalamus. If you have something that opens up the blood-brain barrier, you’re opening the gate. Antibodies are able to come into the brain and find their target.”
Seen in a larger context, a behavioral response to physical ailments makes intuitive sense. When we’re sick with the flu, we feel it, physically and emotionally. We’re listless, down, lack appetite. High fevers, usually signs of extreme inflammation, can cloud thinking and induce hallucinations. “Behavior is the ultimate gauge of what’s going on elsewhere,” says Boris Sakic, a neurologist at Canada’s McMaster University. “If you have the flu, your mood changes. You’re not in the mood to light a cigarette, have chocolate, or make love to your partner.”
Although it’s ordinarily fenced off from the body’s infection-fighting agents, the brain has a complementary system, called microglia, capable of clearing away damaged neurons and fending off infection. Specialized microglial cells make up 10 to 15 percent of the brain. When they go to work, you feel it. Active microglia interfere with neurotransmitters like serotonin, which activates the pleasure sensors in the brain. “That’s why when we have a fever, we feel flat in our mood,” Khandaker says.
Ordinarily, so-called “sickness behavior” is just body and brain working together to fight an infection. Loss of appetite reduces the amount of nutrients available to invasive bacteria; low energy levels let the body route resources to the immune system. As soon as the flu clears up, our mood lifts too.
But when inflammation persists, putting the body and brain in a constant state of alarm, sickness behavior—depression, essentially—can become chronic. Over time, inflammation can do real damage to the brain, as the over-active microglia damage healthy brain cells. “The activation of microglia could be responsible for cognitive decline,” Khandaker says.
Autoimmune diseases like Type 1 diabetes, lupus, arthritis, asthma, and celiac disease are a good model for understanding the link between inflammation, infection, and mental illness. They are some of the most pernicious chain reactions in the body: Immune cells, usually kept busy fighting infections, take aim at the body’s tissues and organs instead, attacking and destroying them with often devastating consequences.
Epidemiological studies have begun to link autoimmune disease to mental illness, supporting the idea that misguided immune reactions can influence the brain. Schizophrenics often have celiac disease, an autoimmune condition of the gut. Lupus, an autoimmune condition that attacks the whole body, sometimes leads to psychotic episodes.
Sometimes the mechanism is even more direct. In her 2012 memoir Brain on Fire, journalist Susannah Cahalan described a precipitous descent into paranoia, psychosis, and violent seizures that landed her in the New York University Langone Medical Center epilepsy ward. She was finally diagnosed with anti-NMDA receptor encephalitis, a rare autoimmune condition that attacks the brain and was first described just seven years ago. After being prescribed steroids, which reduce inflammation, and an immune therapy that attacked the offending antibodies, Cahalan recovered her health.
In 1994, Susan Swedo, a researcher at the National Institute of Mental Health (NIMH) in Bethesda, Maryland, had a hunch that there might be an immunological explanation for obsessive-compulsive disorder. As a model, she was studying a phenomenon known as Sydenham’s chorea, or St. Vitus’ dance.
First described centuries ago, Sydenham’s chorea is a rare manifestation of rheumatic fever that affects children almost exclusively. It is a disconcerting, unmistakable illness to witness. Children are overcome by rapid, uncontrollable jerking of the hands, feet, and face, contorting their bodies in a distorted, disturbing “dance.”
Sydenham’s chorea is caused by molecular mimicry gone wrong. Molecular mimicry generally works like a wolf in sheep’s clothing. Streptococcus bacilli have thrived through the eons by cloaking themselves in proteins that resemble their host’s own cells. Disguised, it evades the immune system just long enough to establish an infection.
But sometimes this tactic sets off an unfortunate chain of events. When the immune system mounts its counterattack, it wipes out the wolf and the sheepskin it’s wearing. In classic rheumatic fever, the antibodies mistake the lining of the heart for strep bacilli. In Sydenham’s, the basal ganglia have a particularly fleece-y look. That, in turn, helps explain an afflicted child’s odd motions. The basal ganglia are walnut sized areas of the brain that serve as a sort of traffic light, signaling the muscles in the proper order to make voluntary movements.
When the basal ganglia are damaged or attacked, the disruption can be severe—as though the traffic light was permanently stuck on green. Everything from Parkinson’s and cerebral palsy to attention deficit hyperactivity disorder (ADHD) have been connected to damaged basal ganglia. “The basal ganglia are the gatekeeper between the brain stem and motor function and the upper brain. They say ‘stop, go, stop, go,’ ” says Swedo. “When they don’t work right, think of the gate as stuck open in certain areas—it’s a failure to inhibit the motor impulse in blinking or twitching.”
Just as puzzling are kids who don’t get PANDAS. That’s led to more than a decade of debate over whether it exists at all.
As Swedo collected case histories of children with OCD, Swedo began to notice remarkable parallels with Sydenhams.’ Most cases of OCD come on slowly, with tics accumulating and intensifying over months and years. But in about a quarter of the childhood-onset OCD cases Swedo looked at, the compulsive behavior came on like a light switch, going from normal to severe overnight. It was often accompanied by tics, like throat clearing and grunting; severe separation anxiety; bed-wetting; and changes in handwriting as fine motor control broke down.
Like rheumatic fever and Sydenham’s chorea, Swedo found, children whose OCD, tics, separation anxiety, and other symptoms came on suddenly often had strep infections not long before their first symptoms appeared. If strep could cause Sydenham’s, she wondered, could it also be affecting kids’ thoughts and behavior? In a 1998 paper, she proposed a link between strep, OCD, and the other symptoms she was seeing, calling the phenomenon “pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections,” or PANDAS.
Isak McCune’s experience is typical of PANDAS. In classic autoimmune diseases like Type 1 diabetes or lupus, the immune system spontaneously mistakes cells in the body for invaders. In PANDAS and Sydenham’s chorea, Swedo says, the attack is set off by an actual infection. As long as the immune system senses strep in the body, it produces antibodies tailored to fight the bacteria.
In people with PANDAS, though, the antibodies slip through the blood-brain barrier to attack similar-looking proteins on the cells of the basal ganglia. “The antibodies are somewhat sloppy; they cross-react with other proteins and chemicals,” says Hornig. “That can lead to changes in behavior or the brain.”
When it comes to treatment, the presence of strep antibodies in the blood of children with OCD is a positive sign. Remove the infection, and the crippling behaviors often go away, too. Once their bodies stand down from the fight against strep, the “cross-reactive” attacks on the basal ganglia seem to stop as well.
Artificially dampening the immune system seems to work in a similar way. Tricia Lord, a California parent whose son Kirk was treated for PANDAS in 2011 with steroids, an immunosuppressant, says she saw improvement within hours. “He was back to what he was before all this happened,” Lord says. “I couldn’t believe it. He seemed better than 100 percent.” (Kirk relapsed after a month, and doctors tried intravenous immunoglobulin, a procedure, designed to regulate the immune system, that infuses patients with antibodies extracted from healthy donors.1 He’s now off all medications and performing above his grade level.)
Much remains mysterious, Swedo says, about the symptoms of PANDAS. One of her early PANDAS cases was a 12-year-old girl convinced she caught rabies from an unopened hypodermic needle she found in her pediatrician’s parking lot. At the age of 5, Kirk Lord developed severe separation anxiety almost overnight, and sunk into a listless state his parents dubbed “the Fog.” Other kids afflicted with PANDAS hear voices or experience “Alice in Wonderland” syndrome, wildly distorted perceptions of size and distance some liken to waking nightmares. “Why is it rabies, or AIDS, or spearmint gum? Some are so random you scratch your head,” Swedo says.
Just as puzzling are the kids who don’t get PANDAS. Strep can be dangerous, but it’s a common part of childhood. The average grade school student comes down with strep twice a year, according to the National Institutes of Health. Yet 1,999 out of 2,000 don’t develop PANDAS. And Swedo estimates that PANDAS accounts for just 10 or 20 percent of all pediatric-onset OCD cases.
That’s led to more than a decade of debate over whether PANDAS exists at all. When Swedo and her colleagues first published their PANDAS results, there was a backlash from Harvey Singer, a professor of neurology and pediatrics at Johns Hopkins University, and Tourette’s researchers, who questioned the idea that a common childhood illness caused tics and OCD. In an influential 2011 Journal of Pediatrics paper, Singer called the evidence that links strep to PANDAS “inconclusive.”
Today Singer says that attempts in numerous studies to confirm the immune system as the “underlying mechanism in PANDAS have been equivocal.” As a result, he and other doctors say the diagnosis isn’t strong enough to justify giving kids powerful courses of antibiotics, let alone treatments like intravenous immunoglobulin, or plasmapheresis, a blood-filtering process typically used to treat severe autoimmune diseases like lupus. Treatments and medications for OCD and ADHD already exist, they say, and should be enough.
Swedo agrees that traditional treatments—cognitive behavior therapy, for example—are part of the solution. “But if you culture for strep and treat early, you can abort the entire disease process,” she says. “That’s one of the reasons this controversy has been so painful.”
Since Swedo’s 1998 paper, researchers have used MRI scans to show enlarged, inflamed basal ganglia in the brains of kids with PANDAS. They’ve swabbed slices of monkey brain with strep cultures taken from PANDAS patients, and observed immediate reactions in the equivalent of basal ganglia tissue. The immediate response to antibiotics and immune-suppressants underscored the connection between the compulsions and volatility of children with PANDAS and their strep infections.
Swedo and her colleagues realize that mental disorders caused directly by infection or autoimmune reaction are the exception rather than the rule. “Not everybody who gets strep ends up with this autoimmune response,” says Hornig. “The majority of people are walking around with anti-brain antibodies, but are perfectly healthy. How can that be?”
The answer is that, as appealing as the “one bacteria, one reaction, one cure” model of mental illness may be, most cases can’t be explained by looking at the immune system alone. Both advocates and critics of PANDAS agree that mental disorders like OCD, depression, or schizophrenia, in children and adults, should be looked at as a set of symptoms with a variety of possible causes. Genes, environment, and immunity all interact in ways doctors are just beginning to unravel.
As doctors and scientists return to an earlier, holistic understanding of the relationship between body and brain, they are potentially gaining new treatments for terrifying illnesses. Knowing that at least some mental disorders are caused by infection puts a new set of tools at doctors’ disposal. Swedo, who today is chief of the Pediatrics and Developmental Neuroscience Branch at NIMH, says this new thinking offers tremendous hope. “The most important fact is just because we don’t know what caused it doesn’t mean it’s not real, and it’s not in the brain,” she says.
Andrew Curry is a journalist in Berlin, Germany. He has written for a wide range of publications, including Archaeology, Discover, National Geographic, and Wired. You can follow him on Twitter @spoke32
Additional Reading
Bernstein, G.A., Victor, A.M., Pipal, A.J., & Williams, K.A. Comparison of clinical characteristics of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections and childhood obsessive-compulsive disorder. Journal of Child and Adolescent Psychopharmacology 20, 333–340 (2010).
Garvey, M.A., Giedd, J., & Swedo, S.E. PANDAS: The search for environmental triggers of pediatric neuropsychiatric disorders. Lessons from rheumatic fever. Journal of Child Neurology 13, 413-423 (1998).
Khandaker, G.M., et al. Inflammation and immunity in schizophrenia: Implications for pathophysiology and treatment. The Lancet Psychiatry 2, 258–270 (2015).
PANDAS: Frequently asked questions about Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections, National Institute of Mental Health, http://www.nimh.nih.gov/health/publications/pandas/index.shtml.
Singer, H.S., Gilbert, D.L., Wolf, D.S., Mink, J.W., & Kurlan, R. Moving from PANDAS to CANS. The Journal of Pediatrics 160, 725–731 (2011).
Swedo, S.W., et al. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: Clinical description of the first 50 cases. American Journal of Psychiatry 155, 264-271 (1998).
Swedo, S.E., Leckman, J.F., & Rose, N.R. From research subgroup to clinical syndrome: Modifying the PANDAS criteria to describe PANS (Pediatric Acute-onset Neuropsychiatric Syndrome). Pediatrics & Therapeutics 2, 1000113 (2012). Retrieved from doi: 10.4172/2161-0665.1000113.
Tsay, C.J. Juius Wagner-Jauregg and the legacy of malarial therapy for the treatment of general paresis of the insane. Yale Journal of Biology and Medicine 86, 245-254 (2013).